A 50 year old male with acute abdomen
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
CONSENT WAS GIVEN BY BOTH PATIENT AND ATTENDER
Chief complaints
A 50 year old male resident of nalgonda presented to opd on 2/1/23 morning with chief complaints of pain Abdomen since 6hours.
History of present illness:
Patient was apparently asymptomatic 6hours then he developed pain Abdomen which was sudden in onset at 12am on 2/1/23 and gradually progressive. Pain was diffuse but more in umbilical and left lumbar region. It was colicky type and non radiating but continuous in nature. History of alcohol intake present. There are no aggravating and relieving factors. No h/o fever, nausea, vomiting and loose stools.
Past history :
Similar complaints in the past 2 years back and was diagnosed as Acute pancreatitis.
Patient is know case of diabetes since 2 years and is on medication. Patient is not a know case of Hypertension, Asthma, tuberculosis, thyroid abnormalities and epilepsy.
Family history: not significant
Personal history:
Daily routine : He wakes up at 8am and does his daily routine and does not go for work and takes 3 meals daily. He drinks alcohol and smokes intermittently through the day and sleeps by 10 pm.
Diet: mixed
Appetite: normal
Sleep : disturbed since 2 days
Bowel and bladder movements: regular
Addictions: Chronic alcoholic since 30 years and takes 180ml per day on an average. Cigarette (tobacco) 2-3 packs daily since 30 years.
Allergies : none
General physical examination:
Patient is conscious, coherent and cooperative. Moderately built and nourished.
Pallor : absent
Icterus : absent
Cyanosis : absent
Clubbing: present
Lymphadenopathy: absent
Edema : absent
Vitals:
Blood pressure: 150/100 mmHg
Pulse rate: 65bpm
Respiratory rate: 20cpm
Temperature: afebrile
Systemic examination:
Abdomen:
Inspection: Abdomen is obese, Umbilicus is central and inverted. All quadrants of Abdomen are moving accordingly with respiration. No visible scars sinuses or engorged veins.
Palpation: All inspectory findings are confirmed. Abdomen is soft and tenderness is present in the umbilical region and left lumbar region. No guarding, no rigidity, no Hepatosplemomegaly and hernial orifices are free .
Percussion: no shifting dullness.
Auscultation: Bowel sounds present.
CVS: S1 S2 present , no murmurs heard
CNS: No focal neurological deficits.
Respiratory system : Bilateral air entry present. Normal vesicular breath sounds heard.
Provisional diagnosis: Acute on chronic pancreatitis secondary to alcohol intake
Investigations:
HAEMOGRAM:
Serum amylase:
Serum lipase:
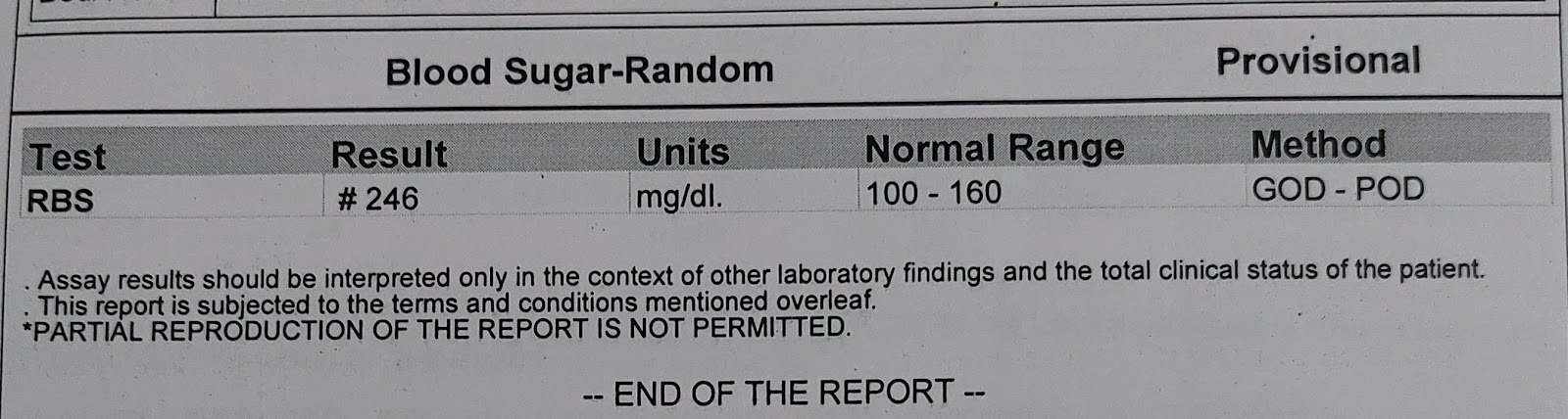
Random blood glucose :
Serum creatinine:
liver function tests: complete urine examination: USG : 2D ECHO: CT SCAN:Treatment:
-NBM
- IV fluids : NS and RL ( 100ml/hr)
-Inj pantop 40mg IV OD
-Inj Thiamine 200mg in 100ml NS iv tid
- Inj HAI s/c tid premeal.
- BP, PR, RR, temperature monitoring and charting 4th hourly.

















Comments
Post a Comment